Visual Comparison of Provider Representation
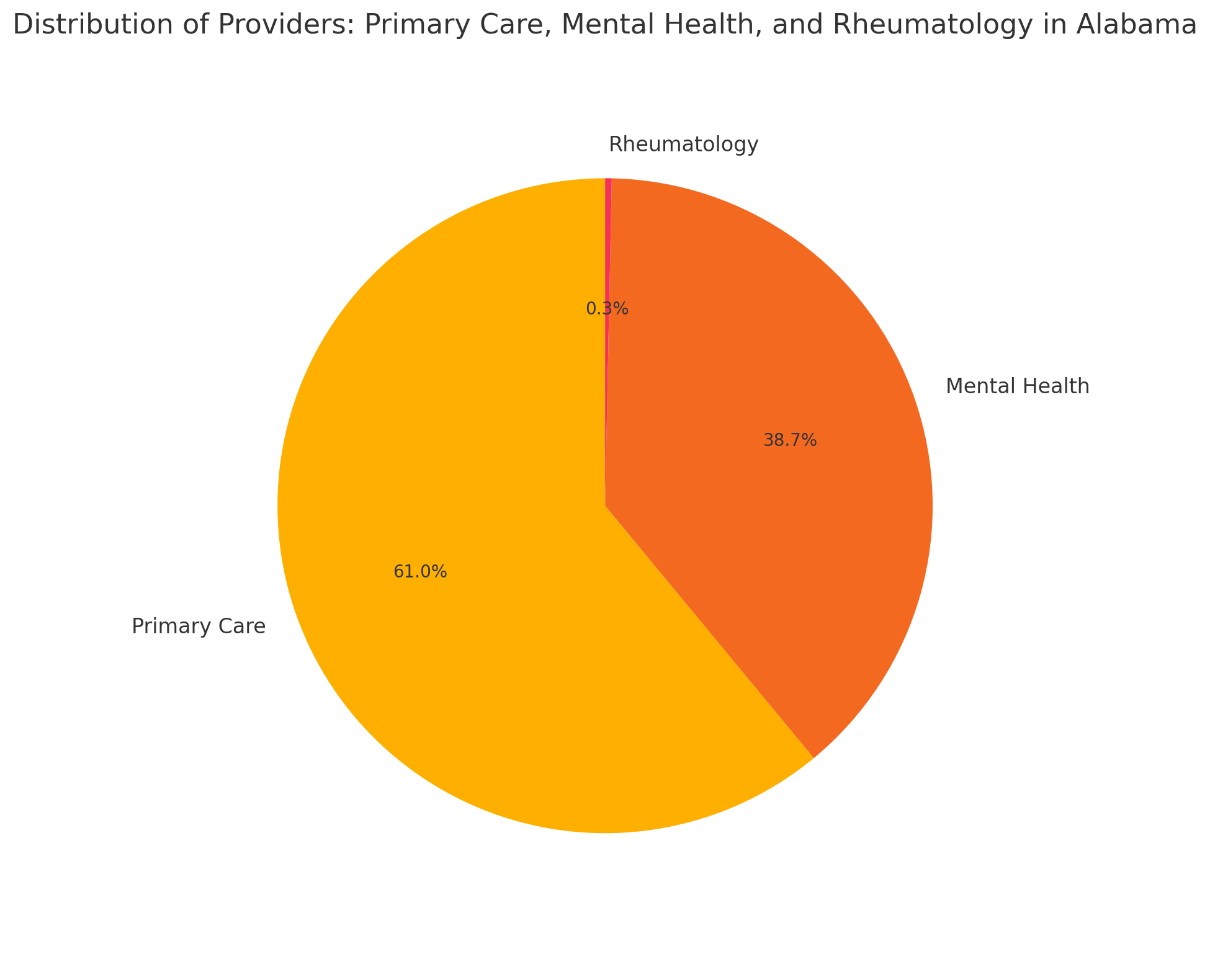
This visual highlights that rheumatology comprises less than 1% of all providers in Alabama — despite widespread chronic need and geographic barriers to access.
Across the U.S., millions of patients with autoimmune and musculoskeletal conditions face long delays or complete lack of access to rheumatologic care. This crisis is deepening as the number of practicing rheumatologists declines due to retirement and burnout, while demand continues to rise—especially in rural areas.
In Alabama and other underserved states, nurse practitioners are increasingly stepping in to fill this gap. Despite this, workforce incentives and support programs still overlook this vital specialty and its providers.
Rheumatology is just one of many specialties facing workforce shortages. Cardiology, endocrinology, gastroenterology, and other fields are seeing similar trends: reduced access, rural underservice, and an aging workforce.
We must rethink how support programs are structured, ensuring all specialty providers in underserved areas are supported—not just those in primary care. This is essential for a truly equitable healthcare system.
| Specialty | Estimated Providers | Ratio (Residents per Provider) |
|---|---|---|
| Primary Care | ~12,000 | ~417:1 |
| Mental Health | ~7,610 | ~657:1 |
| Substance Use Disorder | ~143 facilities | ~34,965:1 |
| Rheumatology | ~64 | ~78,125:1 |
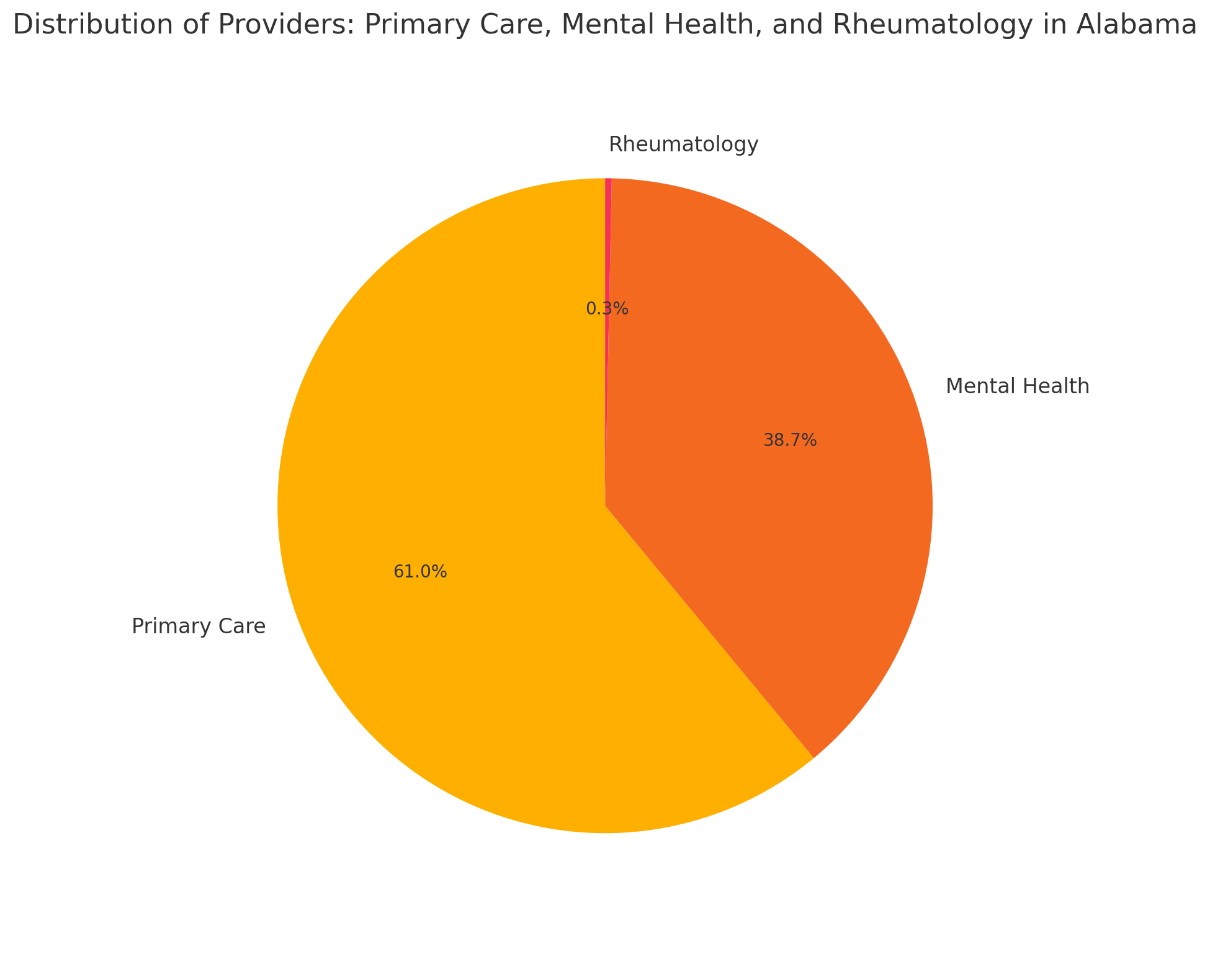
This visual highlights that rheumatology comprises less than 1% of all providers in Alabama — despite widespread chronic need and geographic barriers to access.
Sources: AllTreatment.com, Addiction Resource, PARCA, ADPH